IRD Programs
OPGx-LCA5
LCA5 is an early-onset retinal degeneration that affects approximately 200 people in the U.S. Evidence of a structural-functional dissociation in such individuals suggests an opportunity for therapeutic intervention. OPGx-LCA5 utilizes an AAV vector to deliver a functional LCA5 gene to photoreceptors in the retina. Preclinical data collected in animal and human iPSC models of the disease demonstrated preservation of visual function when OPGx-LCA5 was administered prior to peak disease severity, which suggests a broad therapeutic window for LCA5 patients.
Opus initiated a clinical trial during 2023 with three adult patients with late-stage disease through six months for an OPGx-LCA5 program. This trial has achieved early clinical proof of concept, with new data demonstrating visual restoration in all three patients. Early efficacy and safety data for the first pediatric patients are expected in 2025. For more information, visit clinicaltrials.gov (NCT05616793).
LCA5 is a severe, early-onset form of IRDs. The LCA5 gene encodes for the protein lebercilin, a ciliary protein which is critical for bidirectional protein trafficking in photoreceptor inner and outer segments. Photoreceptors are retinal cells that enable vision by absorbing light and transducing it into an electrochemical signal that is communicated to the visual centers of the brain. In LCA5, the outer segments do not properly develop and photoreceptor function is severely impaired.
OPGx-BEST1
OPGx-BEST1 is being developed for bestrophin-1 (BEST1)-related inherited retinal diseases or bestrophinopathies, a form of macular degeneration found primarily in adults, estimated to affect approximately 9,000 people in the U.S.
Bestrophinopathy is characterized by retinal lesions, with symptoms including dimness of vision, metamorphopsia (distorted vision) or scotoma (blind spot). OPGx-BEST1 leverages an adeno-associated virus (AAV) vector to deliver a functional copy of the BEST1 gene to the retina so that bestrophin-1 protein is produced in retinal pigment epithelial (RPE) cells. This gene therapy approach aims to restore normal function of the RPE cells such that they can provide proper support to photoreceptors, the cells that detect light.
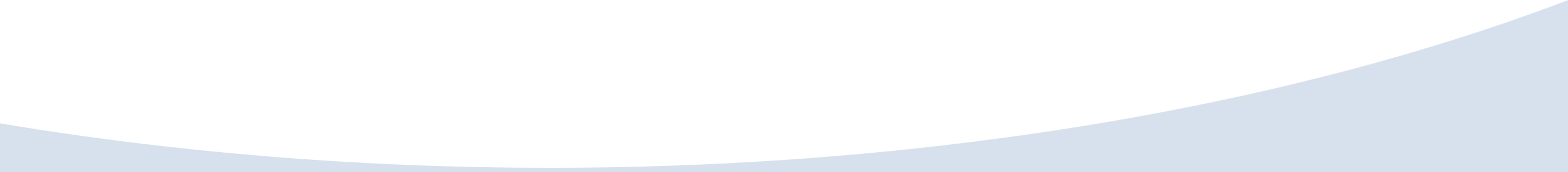
 BEST1 disease is an inherited retinal disease that causes macular degeneration. The BEST1 gene encodes for bestrophin-1, a protein that functions as a retinal pigment epithelial (RPE) cell membrane channel. The BEST1 channel, when activated by calcium (Ca2+) ions, controls chloride (Cl-) ion transfer into and out of the RPE cell. This function is crucial to maintaining homeostasis between rod and cone photoreceptors and RPE cells. Mutations in BEST1 disrupt this homeostasis and result in the breakdown of the rod and cone interphotoreceptor matrix (cIPM) and microvilli (cMV) connection with the RPE. Retinal lesions form containing vitelliform material (“egg-yolk” like) between the RPE and Bruch’s membrane (BM)/choroid (CH). These vitelliform lesions disrupt and cause atrophy of the RPE. Without support from the RPE, photoreceptor cells critical for normal vision die, resulting in progressive vision loss.
BEST1 disease is an inherited retinal disease that causes macular degeneration. The BEST1 gene encodes for bestrophin-1, a protein that functions as a retinal pigment epithelial (RPE) cell membrane channel. The BEST1 channel, when activated by calcium (Ca2+) ions, controls chloride (Cl-) ion transfer into and out of the RPE cell. This function is crucial to maintaining homeostasis between rod and cone photoreceptors and RPE cells. Mutations in BEST1 disrupt this homeostasis and result in the breakdown of the rod and cone interphotoreceptor matrix (cIPM) and microvilli (cMV) connection with the RPE. Retinal lesions form containing vitelliform material (“egg-yolk” like) between the RPE and Bruch’s membrane (BM)/choroid (CH). These vitelliform lesions disrupt and cause atrophy of the RPE. Without support from the RPE, photoreceptor cells critical for normal vision die, resulting in progressive vision loss.
Opus aims to obtain preliminary data from a Phase 1/2 study by the first quarter of 2026.
OPGx-RHO
OPGx-RHO is a gene therapy that targets autosomal dominant retinitis pigmentosa caused by RHO mutations (RHO-adRP). RHO-adRP affects approximately 5,600 people in the U.S., making it one of the most common IRDs.
Encoded by the RHO gene, rhodopsin is an important component of the photopigment in rod photoreceptors that absorbs light and provides structure to the rod outer segment. Autosomal dominant mutations in rhodopsin cause RHO-adRP, which is characterized by progressive death of rod photoreceptors that can lead to vision loss. OPGx-RHO is designed to preserve rod photoreceptors by replacing a patient’s RHO gene with a functional copy of the gene.
OPGx-RHO is in preclinical development to support the initiation of a first-in-human trial in 2026.
OPGx-RDH12
OPGx-RDH12 focuses on restoring protein expression and halting functional deterioration in patients with retinal dystrophy caused by mutations in the retinal dehydrogenase (RDH12) gene.
Patients with RDH12 mutations, which affect approximately 1,100 people in the U.S., often have early visual acuity loss with retinal structural changes by two years of age, and longitudinal studies have reported a steep decline in visual acuity within the second decade of life. OPGx-RDH12 leverages AAVs to transport a functional gene to photoreceptors in the retina. Preclinical studies of OPGx-RDH12 in cellular and mouse models have demonstrated functional improvement of RDH12 activity in mice with mutations in this gene.
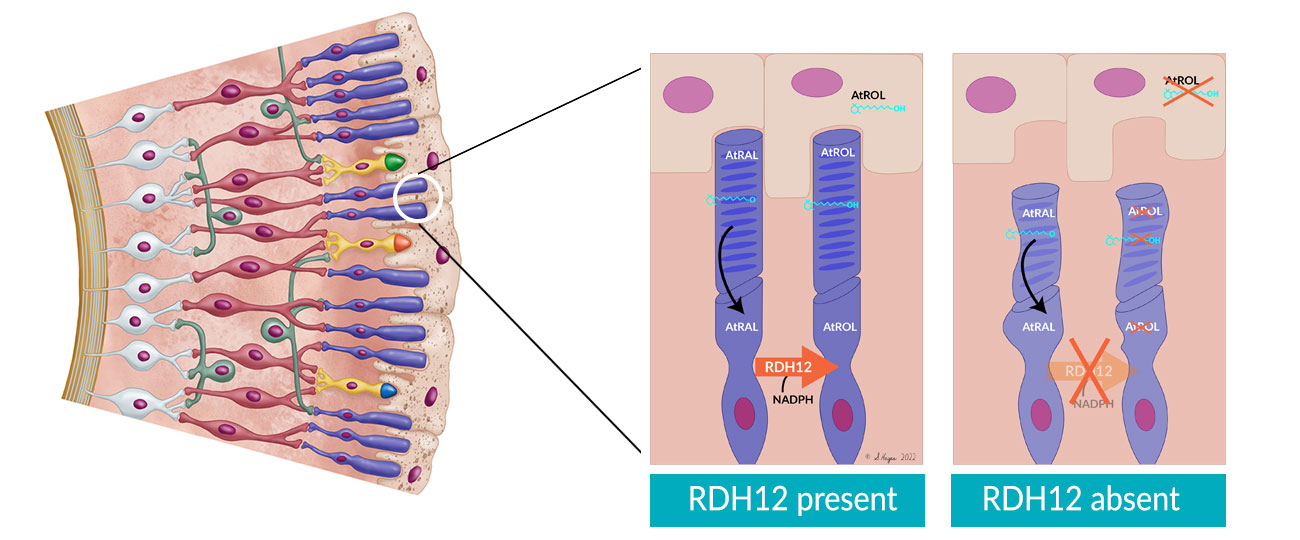
RDH12 is a severe, early-onset IRD. The RDH12 gene encodes for a retinol dehydrogenase enzyme produced in the photoreceptor inner segment that has a key role in the visual cycle. Conversion of all-trans retinal (AtRAL) to all-trans retinol (AtROL) by RDH12 during the visual cycle protects photoreceptors from cytotoxicity. Mutations in RDH12 permit a toxic accumulation of AtROL, leading to photoreceptor degeneration.
OPGx-MERTK
Mutations in the MERTK gene cause a rod-cone dystrophy with early macular atrophy, with retinitis pigmentosa being the most common phenotype. Preclinical studies have shown proof of concept in rats and mice and an early clinical trial with an AAV vector was carried out several years ago with mixed results. Opus is developing OPGx-MERTK as a modern AAV vector for the treatment of MERTK IRD, which affects approximately 600 people in the U.S.
OPGx-NMNAT1
OPGx-NMNAT1 is a gene augmentation therapy designed to halt functional deterioration in pediatric patients with retinal degenerative disease caused by mutations in the nicotinamide mononucleotide adenylyltransferase 1 (NMNAT1) gene, which affects approximately 800 people in the U.S.
NMNAT1 is an enzyme required for regenerating an essential metabolite, nicotinamide adenine dinucleotide (NAD+), in cell nuclei. Photoreceptors, in particular, are highly vulnerable to loss of NMNAT1 function. Preclinical data in a mouse model exhibiting key features of the human disease demonstrated the potential for OPGx-NMNAT1 delivered via AAV to stabilize disease progression.
OPGx-CNGB1
OPGx-CNGB1 is an AAV gene therapy being developed for a late onset form of retinitis pigmentosa due to mutations in the CNGB1 gene, which affects approximately 400 people in the U.S. Opus is collaborating with an NIH funded consortium of university researchers and the Foundation of the NIH’s Bespoke Gene Therapy Consortium to bring this therapy into and through a Phase 1 clinical trial.